Breastfeeding Essentials - Basics for Successful Nursing

Breastfeeding is a natural and beautiful way to nourish your baby, providing them with essential nutrients and building a strong bond between mother and child. However, for many new moms, breastfeeding problems could arise, which can seem daunting and overwhelming. In this basic guide, we will cover the breastfeeding essentials, from understanding how much milk your baby needs to the benefits of breastfeeding for both baby and mother. We will also delve into the differences between colostrum and breast milk, discuss what happens during the first few feedings, and address potential complications for both baby and mother.
How Much Milk Does My Baby Need?
How Is Milk Made?
How do colostrum and breast milk differ from each other?
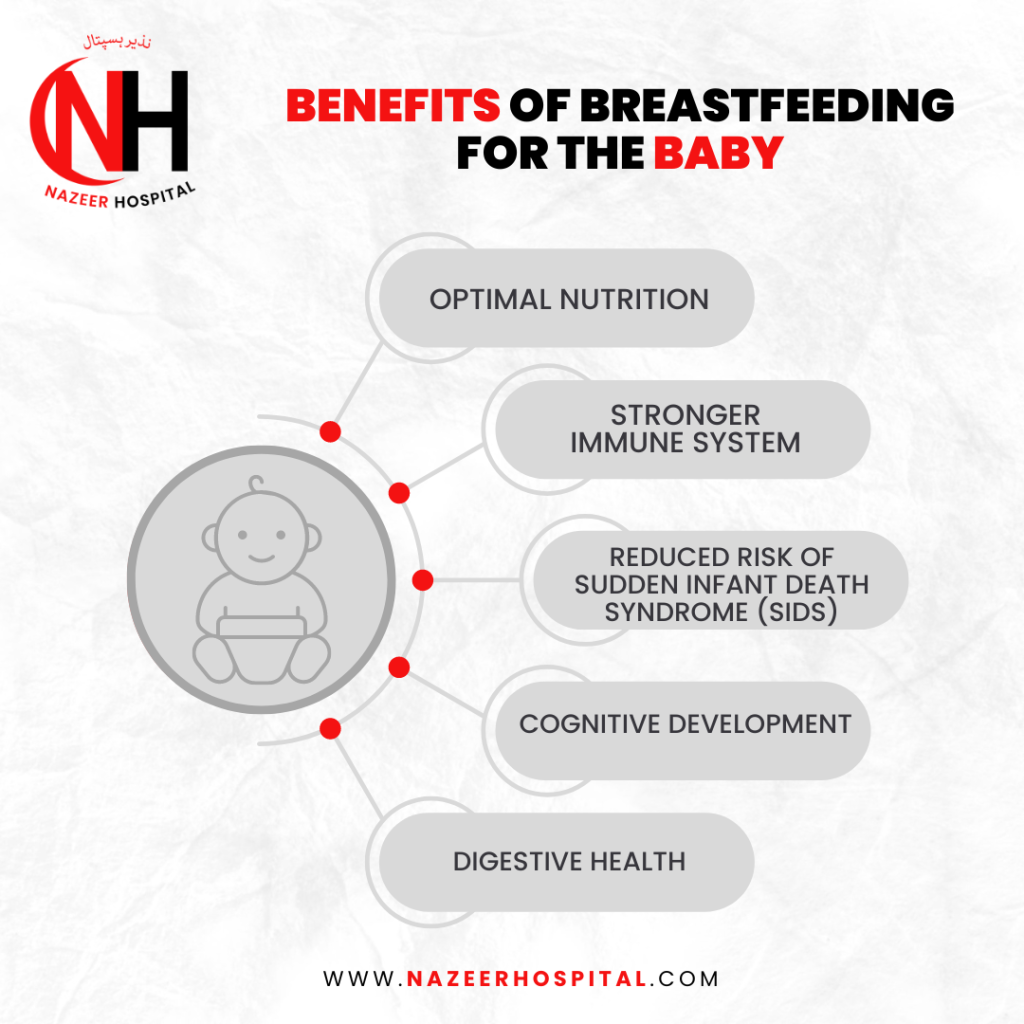
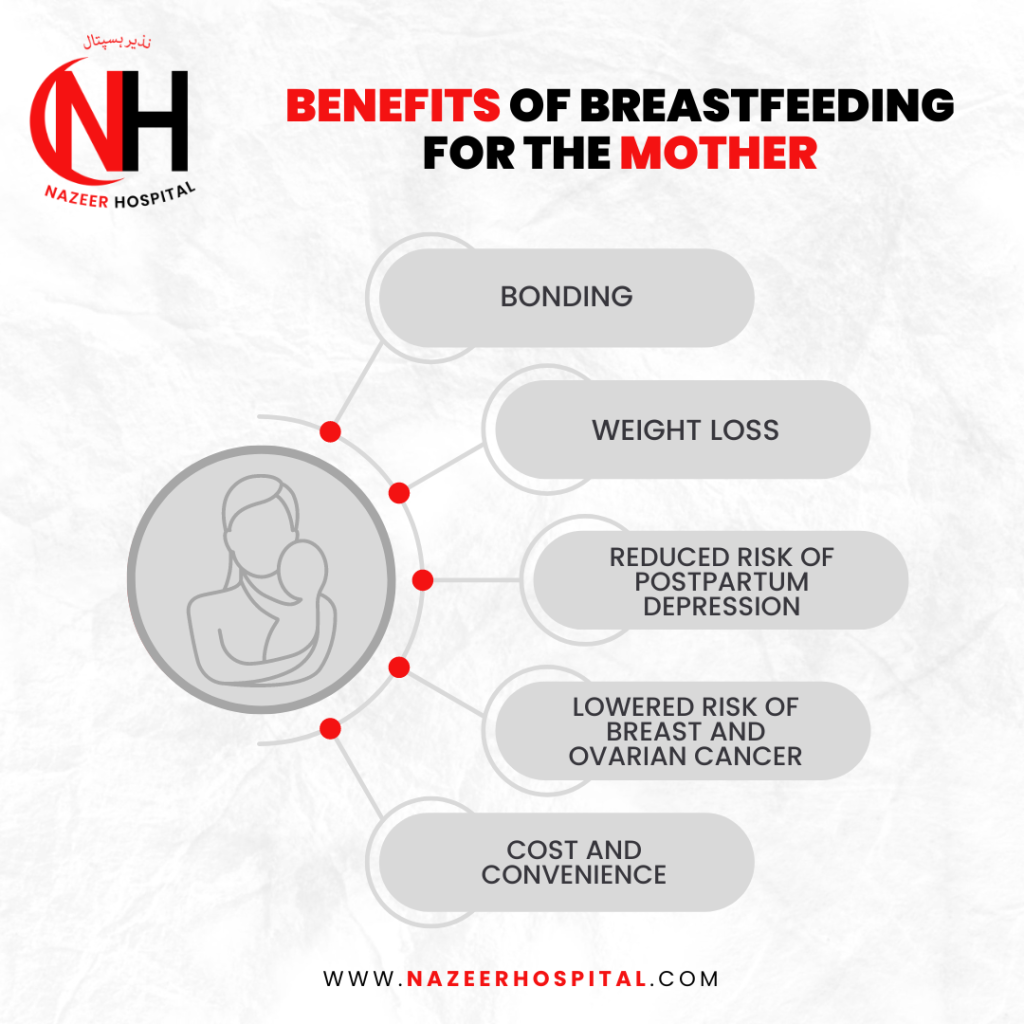
Benefits of Breastfeeding
What Happens During the First Few Feedings?

How Does Nazeer Hospital Support Breastfeeding?
Nazeer Hospital recognizes the importance of breastfeeding essentials and offers comprehensive support to new mothers. Our lactation consultants provide guidance and education on breastfeeding essentials and basics, techniques, latching, and positioning. We also offer assistance in addressing any complications or challenges that may arise during the breastfeeding journey.
Conclusion
By paying attention to the fundamentals of breastfeeding essentials and understanding your baby’s cues, you can ensure a good milk supply. This process can be performed smoothly, providing maximum benefits to the infant while minimizing discomfort for the mother. Although complications may arise, seeking support and guidance from professionals like lactation consultants can help overcome challenges and ensure a successful breastfeeding essential experience. With the support of Nazeer Hospital, breastfeeding mothers receive the necessary care and assistance to make their breastfeeding journey rewarding and fulfilling.
Frequently Asked Questions
The process of breastfeeding typically involves four stages, which are often referred to as the “four stages of lactation.” These stages describe the changes in breast milk production and the feeding patterns of both the mother and the baby. Here are the four steps:
- Colostrum: Colostrum, the initial type of breast milk, is produced during the early days after childbirth. It is thick, yellowish, and rich in nutrients and antibodies. Colostrum helps in providing essential nutrients and immune protection to the newborn. Typically, this phase lasts a few days.
- Transitional Milk: After the colostrum stage, the breasts produce transitional milk. Mature milk and colostrum combine to form transitional milk. It is more abundant in volume than colostrum and contains more fat, lactose, and calories. This stage typically lasts for about two weeks.
- Mature Milk: Around two weeks after childbirth, the breasts produce mature milk. Mature milk is the primary milk supply for the baby throughout the breastfeeding journey. It consists of thinner foremilk, which quenches the baby’s thirst, and hindmilk, which is creamier and higher in fat, providing essential calories and nutrition. This stage continues as long as the mother continues to breastfeed.
- Weaning: The final stage of breastfeeding is weaning, which marks the end of exclusive breastfeeding and the introduction of solid foods or other sources of nutrition. Weaning can be a gradual process, with the baby gradually reducing breast milk intake and incorporating different foods into their diet. The timing and method of weaning vary for each mother-baby pair and depend on individual circumstances and preferences.
Following the first six months, the introduction of complementary foods occurs gradually while breastfeeding is sustained. Breastfeeding can still play an essential role in the baby’s nutrition, and the WHO recommends continued breastfeeding up to two years of age or beyond, alongside appropriate complementary feeding.
- Maternal Medications: Some medications can pass into breast milk and may harm the baby.
- Maternal Illness: Certain contagious illnesses, such as HIV, active tuberculosis, or untreated human T-cell lymphotropic virus type 1 (HTLV-1), can be transmitted through breast milk.
- Substance Abuse: If a mother uses illicit drugs or excessive alcohol, breastfeeding may need to be avoided or limited to protect the baby’s health and well-being.
- Galactosemia: In rare cases, if a baby is diagnosed with galactosemia, a genetic disorder that affects the ability to digest galactose (a sugar present in breast milk), breastfeeding may need to be avoided.
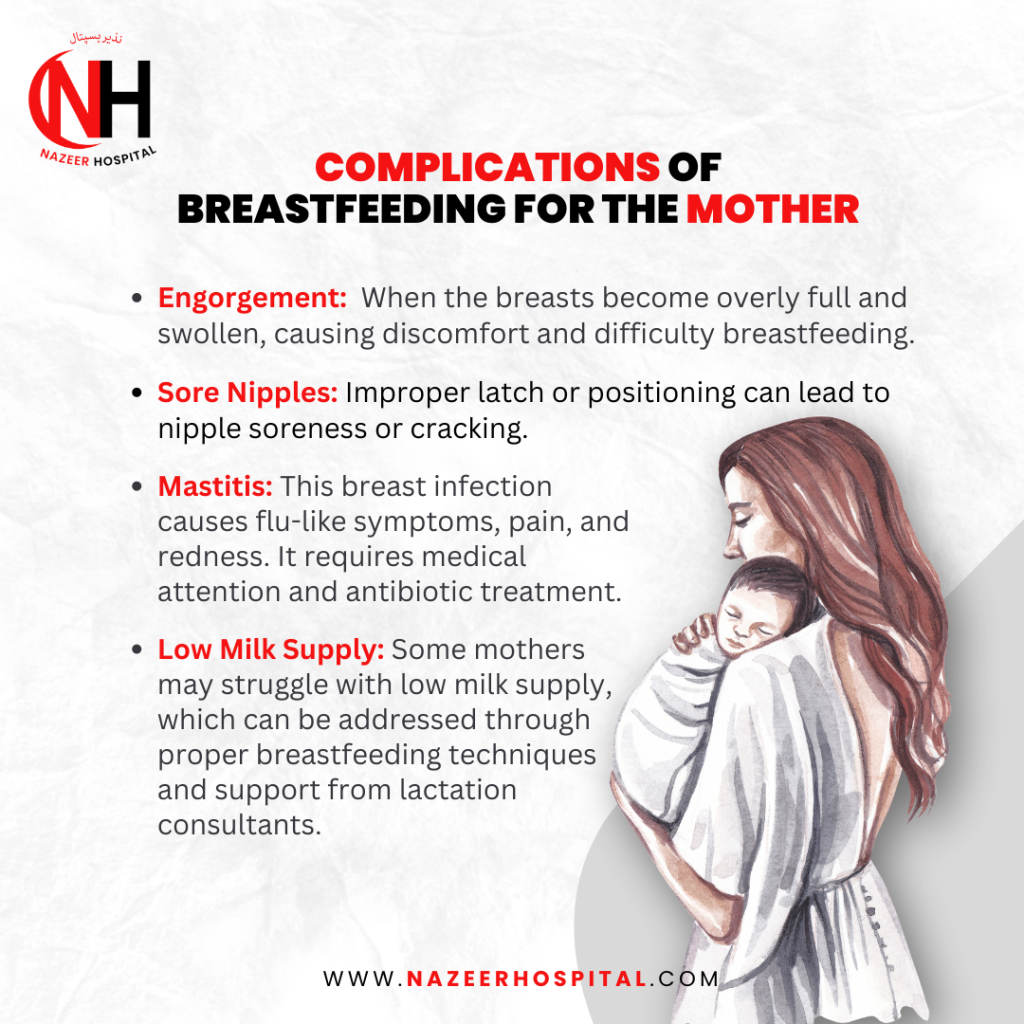
- Breast Infections: In cases of severe breast infections, such as untreated mastitis or abscesses, healthcare professionals may recommend a temporary cessation of breastfeeding from the affected breast until the condition is treated.
It’s important to note that even partial breastfeeding can offer health benefits to both the mother and the baby. The decision to continue breastfeeding beyond the recommended guidelines depends on various factors, including the mother’s and baby’s health, preferences, and circumstances.
- Transmission of Infections: Breast milk can carry infectious agents, such as viruses or bacteria, from the mother to the child. If the donor mother has a contagious condition or is unaware of her health status, she is likely to transmit infections to the receiving child.
- Allergic Reactions: Each mother’s breast milk composition is unique and tailored to meet the specific needs of her baby. Introducing another mother’s breast milk may expose the receiving child to different proteins and substances their body may not tolerate, potentially leading to allergic reactions or gastrointestinal issues.
- Medications and Substances: Breast milk can contain medicines, substances, or even traces of substances consumed by the donor’s mother. These substances may not be suitable for the receiving child and could adversely affect their health and development.
- Unknown Factors: Without proper screening and testing, there may be unknown factors or health conditions of the donor mother that could impact the safety and suitability of her breast milk for another child.
Breastfeeding or skin-to-skin contact before, during, and after vaccine injections has reduced distress and pain responses in infants. The sucking action involved in breastfeeding can activate a baby’s natural calming reflexes and help distract them from the momentary discomfort of the injection.
Additionally, breastfeeding releases endorphins in both the mother and the baby, which can contribute to a sense of well-being and help alleviate pain.
- Freshly Expressed Breast Milk: You can store freshly expressed breast milk in the refrigerator at a temperature of 4°C (39°F) or lower for 4-6 days. Using the milk as soon as possible is recommended to ensure its quality.
- Thawed or Warmed Breast Milk: If you thaw or warm frozen breast milk, it should be used within 24 hours if stored in the refrigerator. Do not refreeze thawed breast milk.
- Leftover Milk from a Feeding: If any breast milk remains in a bottle after a feeding, it is generally safe to refrigerate it and use it within 2 hours. However, it’s important to note that bacteria from the baby’s mouth can enter the bottle during feeding, which may shorten the storage time.
- Store breast milk in clean, sterilized containers with airtight lids.
- Label the containers with the date of expression to keep track of freshness.
- Place the milk towards the back of the refrigerator, where the temperature is most consistent.
- Avoid storing breast milk in the refrigerator door as it may be subject to temperature fluctuations.
- Ensure proper latch and breastfeeding technique: Ensure your baby is latching correctly onto the breast, as a poor latch can affect milk transfer. Seeking guidance from a lactation consultant or breastfeeding counselor can help address any latch issues.
- Breastfeed frequently and on-demand: Frequent and unrestricted breastfeeding can help stimulate milk production. Aim to breastfeed your baby whenever they show hunger cues and allow them to feed for as long as they desire.
- Practice skin-to-skin contact: Skin-to-skin contact with your baby, especially early days, can help stimulate milk production and promote bonding.
- Offer both breasts during feeding: Emptying one breast before switching to the other can ensure that your baby receives the richer hindmilk, which is higher in fat and calories.
- Pumping or hand expressing: Pumping or expressing milk after breastfeeding can help increase milk supply by signaling your body to produce more milk.
- Take care of your well-being: Supporting milk production involves practicing proper self-care, which includes ensuring sufficient rest, maintaining a nutritious diet, and staying well-hydrated.
- Seek support: Contact a lactation consultant, breastfeeding support group, or healthcare professional who can provide guidance and support tailored to your situation.
Dr. Shahzeb Tahir

As an accomplished doctor, I have gained valuable experience working as a House Officer at Al-Nafees Medical College and Hospital. During this period, I underwent a comprehensive internship of one year, which included rotations in various disciplines, such as General Medicine, Dermatology, General Surgery, and Gynae/Obs. This diverse experience has equipped me with a well-rounded perspective on healthcare, enabling me to better understand the complexities of patient care and the diverse needs of individuals.
In addition to my clinical duties, I have taken on the role of an author, writing articles related to medicine and healthcare. I am driven by a passion for spreading awareness and educating the masses on maintaining hygiene, promoting good health practices, and encouraging preventive measures to combat illnesses.

