Gestational Diabetes: How to Keep You and Your Baby Healthy?
Updated on May 3, 2022
Introduction
Gestational diabetes is a type of diabetes that affects women during pregnancy. It occurs when the body cannot produce enough insulin to regulate the increase in blood sugar levels during pregnancy. This condition can cause complications for both the mother and the baby, but with proper treatment, it can be managed effectively.
Definition of Gestational Diabetes
Gestational diabetes is when a woman without previously diagnosed Diabetes develops high blood sugar levels during pregnancy. It is caused by the body’s inability to produce enough insulin to regulate the increase in blood sugar levels that occurs during pregnancy, leading to elevated glucose levels in the blood.
This form of diabetes usually resolves after delivery, but women with gestational diabetes have an increased risk of developing type 2 diabetes later in life. “Gestational age meaning in Urdu” can be referred to as “وقت الحمل”. It measures the duration of pregnancy, calculated from the first day of the last menstrual period.
It is used to monitor the fetus’s growth and development and determine the due date of delivery. Gestational age is an important term used in obstetrics and gynecology to track the progress of pregnancy and to ensure that the mother and fetus receive proper care and monitoring.
What is Gestation?
Gestation refers to the period of pregnancy in mammals, including humans, from the time of fertilization of the egg to the time of birth. It is typically calculated from the first day of the last menstrual period and is usually around 40 weeks or 280 days.
During gestation, the fetus develops and grows inside the uterus, receiving nutrients and oxygen from the mother through the placenta. Gestation meaning in Urdu is “وضع حمل”. It refers to the period from conception to birth when a woman is carrying a fetus in her uterus.
What Is The Gestation Period?
The gestation period is the time between conception and birth during pregnancy. In humans, it usually lasts approximately 280 days, or 40 weeks, from the first day of the last menstrual period. The gestation period is a critical time during which the developing fetus undergoes many changes, including the formation of vital organs and systems. During this time, the mother needs to maintain good health, receive proper care and monitoring, and take steps to reduce potential risks to the developing fetus.
Effects Of Diabetes On Pregnancy
Maternal
Maternal Effects refer to the impact of diabetes on the health of the mother during pregnancy.
Abortion
Women with diabetes are at an increased risk of miscarriage or a still-birth. This may occur due to the abnormal development of the placenta or high blood sugar levels that can affect the growth and development of the fetus.
Preterm Labor
Women with diabetes may be at an increased risk of going into labor prematurely. This can happen due to the overgrowth of the fetus or complications related to diabetes, such as preeclampsia or high blood pressure.
Polyhydramnios
Polyhydramnios is a condition with excess amniotic fluid surrounding the fetus. This can occur in women with diabetes due to the overgrowth of the fetus, which can put pressure on the amniotic sac and cause it to rupture.
Prolonged Labor
Women with diabetes may have more pro-longed labor due to several factors, such as poor uterine contractions, fetal macrosomia (large baby), or a higher incidence of interventions such as induction or cesarean section.
Infections
Women with diabetes may have more pro-longed labor due to several factors, such as poor uterine contractions, fetal macrosomia (large baby), or a higher incidence of interventions such as induction or cesarean section.
Postpartum Hemorrhage
Women with diabetes are at an increased risk of postpartum hemorrhage, excessive bleeding after delivery. This can occur due to poor uterine contractions, retained placenta or placental fragments, or other complications related to diabetes, such as preeclampsia.
Puerperal Sepsis
Puerperal sepsis is a severe bacterial infection that can occur after delivery. Women with diabetes are at an increased risk of developing this infection due to poor glycemic control, which can impair the immune system.
Shoulder Dystocia
Shoulder dystocia is a birth complication where the baby’s shoulder becomes stuck behind the mother’s pelvic bone during delivery. Women with diabetes are at an increased risk of this complication due to fetal macrosomia, which can widen the baby’s shoulders.
Fetal
Fetal effects refer to the impact of diabetes on the health of the fetus during pregnancy.
Macrosomia
Macrosomia is a condition where the baby is larger than average at birth. Women with diabetes are at an increased risk of having a baby with macrosomia due to high blood sugar levels that can lead to excessive fetal growth.
Congenital Malformations
Congenital malformations are birth defects that occur when the fetus is developing in the womb. Women with diabetes are at an increased risk of having a baby with congenital malformations such as heart defects, neural tube defects, and other organ abnormalities.
Birth Injury
Women with diabetes are at an increased risk of having a baby with birth injuries such as nerve damage, fractures, or bruising. This can happen due to the larger size of the baby, which can make delivery more difficult.
Fetal Growth Restriction
Fetal growth restriction is a condition where the baby is smaller than average for its gestational age. Women with diabetes are at an increased risk of having a baby with fetal growth restriction, primarily if the diabetes is poorly controlled.
Stillbirth
Stillbirth is the loss of a baby before delivery after 20 weeks of pregnancy. Women with diabetes are at an increased risk of stillbirth, mainly if the diabetes is poorly controlled. This can occur due to complications such as fetal distress, placental abruption, or umbilical cord problems.
Neonatal
Neonatal effects refer to the impact of diabetes on the health of the newborn baby after delivery.
Hypoglycemia
Hypoglycemia is when the baby’s blood sugar levels are lower than normal. Babies born to women with diabetes are at an increased risk of hypoglycemia due to excessive insulin production in response to the high blood sugar levels during pregnancy.
Respiratory Distress Syndrome
Respiratory distress syndrome is a breathing disorder that occurs in premature babies. Babies born to women with diabetes are at an increased risk of respiratory distress syndrome due to premature delivery or delayed lung development.
Hyperbilirubinemia
Hyperbilirubinemia is a condition with an excess bilirubin in the blood, which can lead to jaundice. Babies born to women with diabetes are at an increased risk of hyperbilirubinemia due to increased red blood cell breakdown or liver dysfunction.
Hypocalcemia
Hypocalcemia is when the baby’s blood calcium levels are lower than normal. Babies born to women with diabetes are at an increased risk of hypocalcemia due to excessive insulin production during pregnancy, which can interfere with calcium regulation.
Hypomagnesemia
Hypomagnesemia is when the baby’s blood magnesium levels are lower than normal. Babies born to women with diabetes are at an increased risk of hypomagnesemia due to increased urinary magnesium excretion and decreased magnesium transfer from the mother.
Polycythemia
Polycythemia is a condition where there is an excess of red blood cells in the blood. Babies born to women with diabetes are at an increased risk of polycythemia due to increased fetal erythropoietin production, which stimulates the production of red blood cells.
These neonatal complications can be managed with proper monitoring and treatment. It is important to closely monitor the baby’s health and blood sugar levels after delivery and provide appropriate care to prevent or manage any possible complications.
Importance of gestational diabetes management
Proper management of gestational diabetes is important for several reasons:
Maternal Health
Uncontrolled gestational diabetes can lead to high blood pressure, excessive weight gain, and an increased risk of complications during pregnancy and delivery.
Fetal Health
High blood sugar levels during pregnancy can increase the risk of macrosomia (large birth weight), birth defects, and stillbirth.
Long-Term Health
Women with gestational diabetes are at a higher risk of developing type 2 diabetes later in life.
Improved Outcomes
With proper management, including a healthy diet, physical activity, and medication if needed, the outcomes for both the mother and baby can be improved.
Therefore, women with gestational diabetes must receive adequate care and support to properly manage their condition and ensure the best possible outcomes for themselves and their babies.

Overview of the article
Causes and Risk Factors For Gestational Diabetes
The exact cause of gestational diabetes is not fully understood, but several factors can increase a woman’s risk of developing the condition, including
Family History of Diabetes
Women with a family history of diabetes, particularly type 2 diabetes, are at an increased risk of developing gestational diabetes.
Being Overweight or Obese Before Pregnancy
Excess weight can increase insulin resistance, making it more difficult for the body to regulate blood sugar levels.
Genetic Predisposition of Diabetes
This is because a family history of diabetes can indicate a genetic predisposition to the condition, which can increase a woman’s likelihood of developing insulin resistance and gestational diabetes during pregnancy.
Previous Gestational Diabetes or Delivery of a Large Baby
Women who have had gestational diabetes in a previous pregnancy or have delivered a large baby (macrosomia) are at increased risk for developing gestational diabetes in future pregnancies.
Having High Blood Pressure
High blood pressure can indicate underlying insulin resistance, which increases the risk of gestational diabetes.
Polycystic Ovary Syndrome (PCOS)
Women with PCOS are at increased risk of developing insulin resistance, which can lead to gestational diabetes.
Race/ethnicity (e.g., Higher Risk in African American, Hispanic/Latino, Native American, and Asian American Women)
Certain racial and ethnic groups, such as African American, Hispanic/Latino, Native American, and Asian American women, are at an increased risk for gestational diabetes.
Advanced Maternal Age (35 Years or Older)
Women who become pregnant at an older age are at a higher risk for developing gestational diabetes.
Impaired Glucose Tolerance or Insulin Resistance
Women with impaired glucose tolerance or insulin resistance are at a higher risk of developing gestational diabetes during pregnancy.
It’s important to note that not all women with these risk factors will develop gestational diabetes, and some women without any of these risk factors may still develop the condition. Regular prenatal care and glucose testing can help identify women at risk for gestational diabetes and allow for prompt treatment.
Symptoms and Diagnosis
The symptoms of gestational diabetes can be subtle and may not be noticeable, so many women do not experience any symptoms. However, some women may experience
Gestational Diabetes Symptoms
Increased thirst, hunger, excessive fatigue, frequent urination, and blurred vision. High blood sugar levels may bring on these signs. Since they can resemble those of other ailments, it is crucial to receive routine prenatal care and glucose testing to keep an eye out for gestational diabetes.
Diagnosis of Gestational Diabetes
Diagnosis of gestational diabetes typically occurs during routine prenatal care, usually between 24 and 28 weeks of pregnancy. However, women who are at increased risk for gestational diabetes, such as those who are overweight or obese, have a family history of diabetes, or have a previous history of gestational diabetes, may be tested earlier.
The main diagnostic test for gestational diabetes is a glucose tolerance test, which measures a woman’s blood sugar levels after fasting and drinking a sugary solution. Women with gestational diabetes typically have elevated blood sugar levels after the sugary drink.
Testing for Gestational Diabetes
The glucose tolerance test for gestational diabetes involves fasting overnight and then drinking a sugary solution. Blood sugar levels are then measured at regular intervals over several hours to determine if they are elevated.
Suppose the results of the glucose tolerance test are abnormal. In that case, a woman may be diagnosed with gestational diabetes and undergo additional testing to monitor her blood sugar levels throughout pregnancy. This can involve regularly checking her blood sugar levels at home using a glucose meter or receiving regular glucose monitoring at a doctor’s office or clinic.
It’s important to note that early diagnosis and treatment of gestational diabetes can help ensure a healthy pregnancy and prevent complications for both the mother and baby. Regular prenatal care and glucose testing are important for all pregnant women to monitor for gestational diabetes. If gestational diabetes is diagnosed, a woman may need to change her diet and engage in regular physical activity to help manage her blood sugar levels and ensure a healthy pregnancy. In some cases, medication may also be necessary to help manage blood sugar levels.
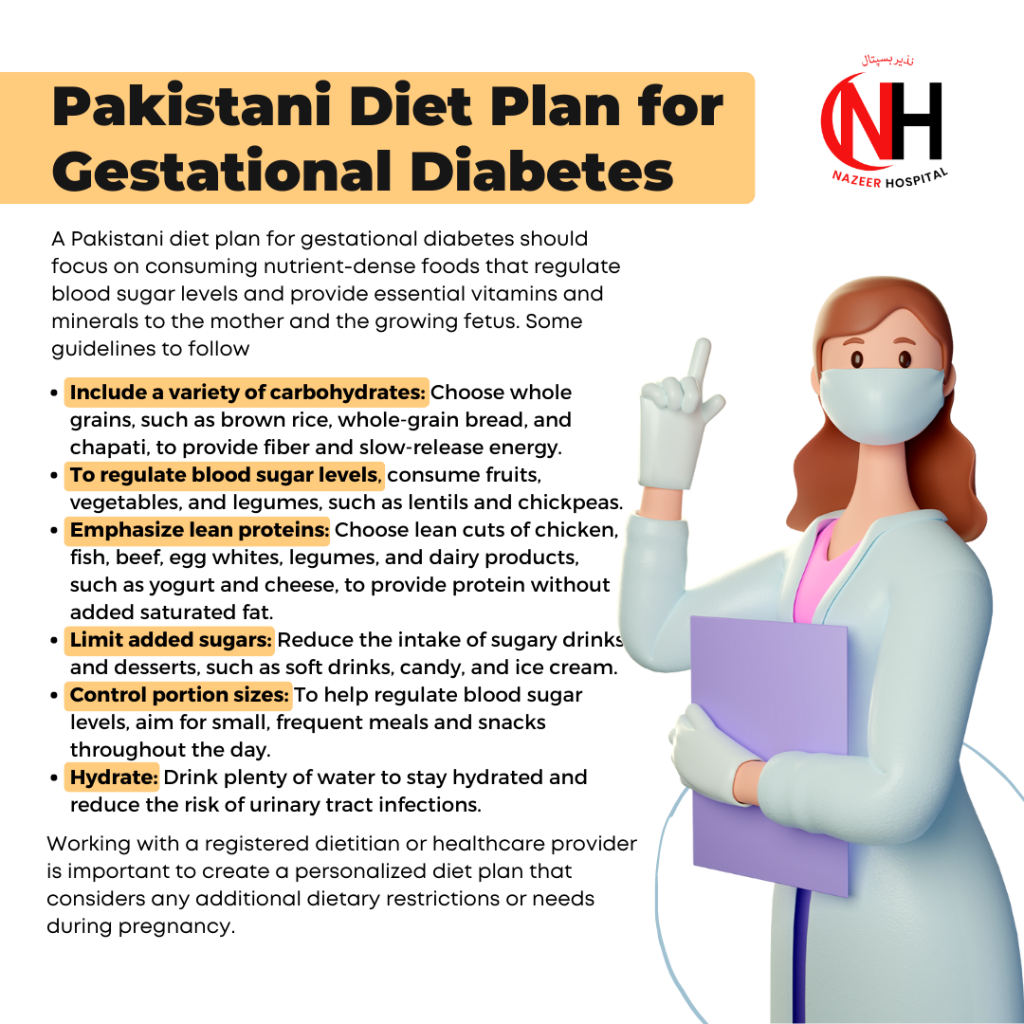
How To Treat Gestational Diabetes Naturally?
The treatment for gestational diabetes in pregnancy and management involve several key components:
Diet and Exercise
Limit Refined Carbohydrates
Foods such as white bread, pasta, and sugar-sweetened beverages can cause rapid spikes in blood sugar levels. Try to limit your intake of these foods and opt for complex carbohydrates, such as whole-grain bread and pasta, instead.
Control Portion Sizes
Eating larger portions can cause your blood sugar levels to rise. Try to control your portion sizes by eating smaller, more frequent meals throughout the day.
Limit Added Sugars
Foods and drinks high in added sugars, such as candy, cakes, and soft drinks, can also contribute to high blood sugar levels. Try to limit your intake of these foods and opt for healthier natural sugar sources, such as fruit.
Incorporate Healthy Fats
The Gestational diabetes diet should include Healthy fats, such as those found in nuts, seeds, avocado, and olive oil, which can help regulate blood sugar levels and improve insulin sensitivity. Try to include these foods in your diet.
Stay Hydrated
Drinking plenty of water can help regulate blood sugar levels and prevent dehydration, making blood sugar control more difficult.
Physical Activity
Regular physical activity, such as walking, can help improve insulin sensitivity and manage blood sugar levels. Aim for at least 30 minutes of moderate-intensity activity, such as brisk walking, most days of the week.
Blood Sugar Monitoring
Monitoring your blood sugar levels regularly is important for managing gestational diabetes. This may involve using a glucose meter to measure your blood sugar levels at home or receiving regular glucose monitoring at a doctor’s office or clinic.
Sugar Level During 8th Month Pregnancy
The blood sugar level during the 8th month depends on various factors such as the woman’s overall health, pregnancy complications, and individual tolerance. However, generally, the target range for fasting blood sugar levels during pregnancy is between 70-99 mg/dL. If you have gestational diabetes, your healthcare provider may recommend more frequent monitoring and specific blood sugar targets. It is important to regularly check blood sugar levels and follow your healthcare provider’s recommendations to ensure a healthy pregnancy.
Normal Sugar Level in Pregnancy
The normal range for blood sugar levels during pregnancy can vary, but generally, a fasting blood sugar level of 70-99 mg/dL is considered normal. However, some healthcare providers may have different targets based on individual circumstances. It’s important to follow your healthcare provider’s recommendations for blood sugar monitoring during pregnancy to ensure a healthy pregnancy outcome. Additionally, it’s important to maintain a healthy diet, exercise regularly, and manage any underlying health conditions to help keep blood sugar levels within the normal range.
Ideal Blood Sugar Level During Pregnancy
The ideal blood sugar level during pregnancy can vary depending on individual circumstances and guidelines set by healthcare providers. However, as a general guideline, the American Diabetes Association (ADA) recommends the following target blood sugar levels for women with gestational diabetes:
- Fasting blood sugar: 95 mg/dL or lower
- One hour after a meal: 140 mg/dL or lower
- Two hours after a meal: 120 mg/dL or lower
It’s important to note that these are general guidelines and your healthcare provider may have different targets based on your individual needs and circumstances. Regular monitoring of blood sugar levels, along with a healthy diet, exercise, and any necessary medications, can help keep blood sugar levels within the recommended range and ensure a healthy pregnancy outcome.
Close Monitoring During Pregnancy
Regular prenatal care is important for the mother and baby’s health. This may involve regular ultrasound scans, prenatal tests, and glucose monitoring to ensure that blood sugar levels are well-controlled and that the pregnancy is progressing smoothly.
Medications
Sometimes, lifestyle changes alone may not be enough to control gestational diabetes effectively. In these cases, medication may be necessary to help manage blood sugar levels. Some commonly used medications for gestational diabetes include insulin and oral hypoglycemic agents. Your healthcare provider will work with you to determine the best treatment plan for your needs.
Monitoring of Blood Sugar Levels
Regular monitoring of blood sugar levels is important in managing gestational diabetes. This may involve self-monitoring blood glucose levels at home using a blood glucose meter and regular visits to a healthcare provider to monitor your overall health and glucose levels.
Collaboration With Healthcare Providers
Collaborating with a healthcare team that includes a doctor, registered dietitian, and other specialists is critical for managing gestational diabetes. This team will work with you to develop a comprehensive treatment plan and provide ongoing support to help you manage your condition. They may monitor you for potential complications and guide a healthy pregnancy and delivery.
It is important to remember that every woman’s experience with gestational diabetes is unique, and the best approach to managing the condition will vary from person to person. It is essential to work closely with your healthcare provider to develop an appropriate plan.
It’s important to work closely with your healthcare provider to develop an individualized treatment and management plan for gestational diabetes. Changing your lifestyle and diet, monitoring your blood sugar levels regularly, and following your healthcare provider’s recommendations can help ensure a healthy pregnancy and prevent complications for both the mother and baby.
Complications
Gestational diabetes can lead to several complications, both for the mother and the baby, if not properly managed. Some potential complications include:
High Birth Weight
Babies born to mothers with gestational diabetes are at higher risk of being larger than average, which can lead to a difficult delivery and an increased risk of injury to the baby.
Risks To The Mother
- Preeclampsia (high blood pressure and protein in the urine during pregnancy)
- Increased risk of cesarean delivery
- Increased risk of type 2 diabetes later in life
Risks To The Baby
- High birth weight (macrosomia)
- Increased risk of birth injury
- Increased risk of hypoglycemia (low blood sugar)
- Increased risk of jaundice
- Increased risk of respiratory distress
Long-Term Risks For The Mother And Baby
1- Preterm labor and delivery: Women with gestational diabetes are at an increased risk of delivering their babies early.
2- Macrosomia: Babies born to mothers with uncontrolled gestational diabetes are at risk of being overweight, a condition known as macrosomia. This can make delivery more difficult and lead to injury to the baby.
3- Increased risk of cesarean delivery: Women with gestational diabetes are at an increased risk of having a cesarean delivery, also known as a C-section.
4- Increased risk of neonatal complications: Babies born to mothers with gestational diabetes are at an increased risk of developing health problems, including hypoglycemia (low blood sugar), jaundice, and respiratory distress.
5- Increased risk of type 2 diabetes: Women with gestational diabetes have an increased risk of developing type 2 diabetes later in life.
6- It is important to work closely with a healthcare provider to manage gestational diabetes and reduce the risk of complications. Regular monitoring and a healthy lifestyle, including a balanced diet and exercise, can help ensure a healthy pregnancy and delivery.
2- Macrosomia: Babies born to mothers with uncontrolled gestational diabetes are at risk of being overweight, a condition known as macrosomia. This can make delivery more difficult and lead to injury to the baby.
3- Increased risk of cesarean delivery: Women with gestational diabetes are at an increased risk of having a cesarean delivery, also known as a C-section.
4- Increased risk of neonatal complications: Babies born to mothers with gestational diabetes are at an increased risk of developing health problems, including hypoglycemia (low blood sugar), jaundice, and respiratory distress.
5- Increased risk of type 2 diabetes: Women with gestational diabetes have an increased risk of developing type 2 diabetes later in life.
6- It is important to work closely with a healthcare provider to manage gestational diabetes and reduce the risk of complications. Regular monitoring and a healthy lifestyle, including a balanced diet and exercise, can help ensure a healthy pregnancy and delivery.
Prevention
To prevent gestational diabetes, it is recommended to
- Maintain a healthy weight before pregnancy
- Eat a healthy diet that is high in fiber, fruits and vegetables, and whole grains and low in added sugars and saturated fat
- Engage in regular physical activity, such as 30 minutes of moderate exercise most days of the week
- Manage any pre-existing health conditions, such as polycystic ovary syndrome (PCOS) or prediabetes
- Avoid excessive weight gain during pregnancy
- Avoid exposure to tobacco smoke
- Get regular prenatal care to monitor your health and the health of your baby
It’s important to note that not all cases of gestational diabetes can be prevented, but following these steps can lower your risk.
Myths and Facts
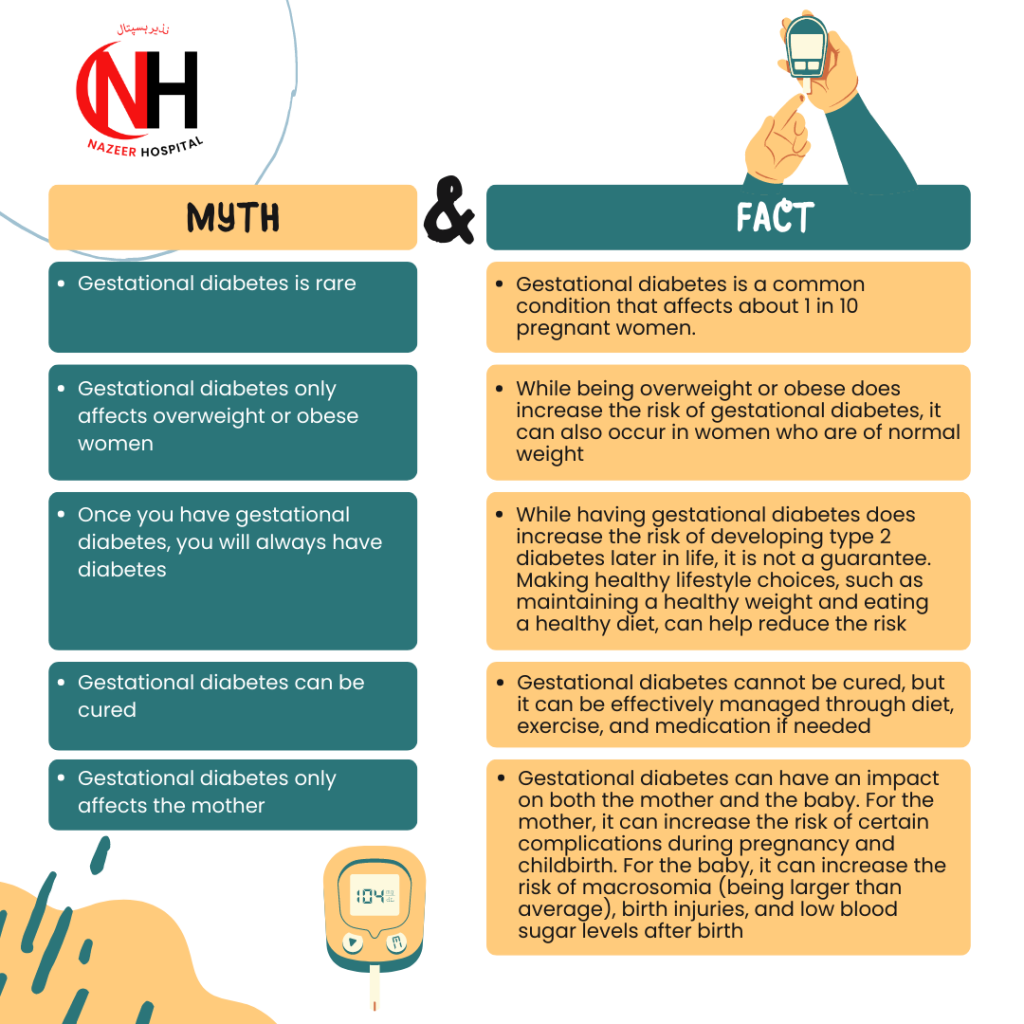
It is important to work closely with your healthcare provider to understand and manage the risks associated with gestational diabetes.
Conclusion
In conclusion, gestational diabetes is a type of diabetes that occurs during pregnancy and affects about 1 in 10 women. Hormonal changes during pregnancy cause it. It is influenced by several risk factors such as family history, overweight or obese, advanced maternal age, and belonging to specific ethnic groups. The condition is diagnosed through blood glucose testing and can be effectively managed through diet and exercise, monitoring blood sugar levels, and, if necessary, medication.
The management of gestational diabetes is important for both the mother and the baby as it can reduce the risk of complications during pregnancy and childbirth. These complications can include pre-eclampsia, macrosomia, and birth injuries for the baby and an increased risk of developing type 2 diabetes for the mother.
It is also essential to be aware of common myths and misconceptions about gestational diabetes, such as the belief that it is rare or only affects overweight women.
If you have been diagnosed with gestational diabetes, it is recommended that you work closely with your healthcare provider to create a management plan that works for you. Organizations such as the American Diabetes Association and the American College of Obstetricians and Gynecologists are excellent resources for more information and support.
Frequently Asked Questions About Gestational Diabetes
Gestational diabetes is a type of diabetes that occurs during pregnancy and affects the way the body uses insulin.
Risk factors for gestational diabetes include being overweight or obese, having a family history of diabetes, advanced maternal age, and belonging to specific ethnic groups.
Gestational diabetes screening is a test that checks a pregnant woman’s blood sugar level to determine if she has gestational diabetes.
Gestational diabetes is typically diagnosed through a blood glucose test between 24 and 28 weeks of pregnancy.
Gestational diabetes can be managed through diet and exercise, monitoring blood sugar levels, and, if necessary, medication.
If gestational diabetes is not properly managed, it can increase the risk of complications during pregnancy and childbirth, such as macrosomia, pre-eclampsia, and birth injuries.
Yes, women with gestational diabetes have an increased risk of developing type 2 diabetes later in life.
Maintaining a healthy weight before pregnancy, eating a healthy diet, and engaging in regular exercise can reduce the risk of developing gestational diabetes.
The American Diabetes Association and the American College of Obstetricians and Gynecologists are excellent resources for more information and support. You can consult your healthcare provider for more personalized information and support.
Dr. Summayya Khalid

M.B.B.S, FCPS (Part 1) – Medicine and Allied
I am Graduated From Foundation University, Islamabad. I have a working experience at Fauji Foundation Hopsital, Rawalpindi and Anwar Hospital, Rawalpindi.
I am fully licensed, highly passionate and determined medical practitioner with a empathetic and professional attitude having strong clinical abilities combined to providing patients with the best care possible. I am skilled in handling paediatric, gynaecological & obstetric emergencies as well.
I also participated in various conferences and seminars and achieved certificates. I am a motivated team leader with strong organization and prioritization abilities, I have organized and participated in health camps in remote areas.
I am fully licensed, highly passionate and determined medical practitioner with a empathetic and professional attitude having strong clinical abilities combined to providing patients with the best care possible. I am skilled in handling paediatric, gynaecological & obstetric emergencies as well.
I also participated in various conferences and seminars and achieved certificates. I am a motivated team leader with strong organization and prioritization abilities, I have organized and participated in health camps in remote areas.


